-
Publish Your Research/Review Articles in our High Quality Journal for just USD $99*+Taxes( *T&C Apply)
Offer Ends On
Tharanikumar Sivakumar*, Abinaya C, Abdul Ajees Meeran M, Nachiappan S, Ashok Prasanna R and Elaveyini U
Corresponding Author: Tharanikumar Sivakumar, Associate Dean, Meenakshi Academy of Higher Education and Research, India.
Received: May 14, 2025 ; Revised: May 26, 2025 ; Accepted: May 29, 2025 ; Available Online: July 08, 2025
Citation: Sivakumar T, Abinaya C, Meeran MAA, Nachiappan S, Prasanna RA, et al. (2025) OPG vs CBCT in Evaluating Difficulty Index of Impacted Mandibular Third Molar Extraction in South Indian Population. J Oral Health Dent Res, 5(1): 1-8.
Copyrights: ©2025 Sivakumar T, Abinaya C, Meeran MAA, Nachiappan S, Prasanna RA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Views & Citations
Likes & Shares
Aim: This study aimed to compare cone beam computed tomography (CBCT) and orthopantomogram (OPG) in assessing mandibular third molar impactions and their relationship with the inferior alveolar nerve (IAN) canal in South Indian population.
Methods: The study compared OPG & CBCT images from 254 individuals aged 18-45 years with unilateral or bilateral mandibular third molar impaction, was evaluated for the effectiveness in identifying key parameters, including mandibular height, second molar angulation, and canal placement.
Result: CBCT demonstrated higher accuracy than OPG, particularly for assessing mandibular canal position and cases in specific angulation ranges (70-79 degrees). CBCT also identified more cases of distal cusp coverage and available space for impacted teeth compared to OPG. While root morphology and follicular diameters showed no significant differences between imaging methods, a statistically significant association was found between mandibular height and canal location (p-value <0.05). CBCT achieved a mean score of 4.58, reflecting its enhanced precision in complex cases such as impacted third molars. The findings emphasize CBCT’s superiority in providing detailed anatomical information essential for surgical planning, reducing the risk of iatrogenic damage to critical structures like the IAN during mandibular third molar extractions.
Conclusion: The study concludes that CBCT is a more effective diagnostic tool than OPG for preoperative assessment, particularly in cases where precise anatomical relationship visualization is necessary, and recommends further research to improve preoperative assessments and reduce extraction complications.
Keywords: Mandibular Third Molar Impaction, Cone Beam Computed Tomography (CBCT), Orthopantomogram (OPG), Inferior Alveolar Nerve (IAN), Preoperative Assessment
INTRODUCTION
An impacted tooth is a tooth that remains fully or partially unerupted, positioned against another tooth, bone, or soft tissue, making its future eruption uncertain [1]. Factors influencing the eruption of third molars include genetic inheritance, diet-related attrition, decreased mesiodistal crown diameter, and the use of masticatory apparatus [2]. Studies suggest women are more likely than men to experience mandibular third molar impaction [3].
Third molar extractions pose a risk of iatrogenic injury to the inferior alveolar nerve (IAN). The nerve’s complex anatomy-its path, shape, and direction-often complicates assessments, making precise preoperative planning challenging [4]. Understanding the proximity of impacted third molars to the inferior alveolar canal is crucial to prevent nerve injury during surgery [5].
While the anatomy of the IAN and surrounding structures has been studied, certain limitations exist. Cadaveric studies may not generalize to living patients due to differences in age or pathology. Skull-based studies often lack demographic data or rely on inconsistent anatomical landmarks. Additionally, two-dimensional imaging modalities and conventional CT scans have inherent limitations, including poor accuracy in assessing nerve positioning [6].
This study aimed to fill the gap in research on the South Indian population by investigating the relationship between the inferior alveolar canal (IAC) and mandibular molars. Specifically, it examined the proximity of the canal to molar periapices, assessed cortical thickness, and compared these parameters for second and third molars using cone beam computed tomography (CBCT) and OPG.
CBCT offers superior visualization of the mandibular canal compared to OPG, making it a valuable tool for reducing nerve injury risks during odontectomy procedures.
STUDY OBJECTIVES
CBCT provides more detailed and accurate visualization of the IAC compared to OPG, especially in cases of cortical decortication where nerve injury risks are higher. This study aims to support the safer extraction of impacted mandibular third molars by emphasizing the need for advanced imaging techniques in preoperative evaluation.
MATERIALS AND METHODS
This observational study was conducted in the dental clinic of Sathyabama University, Chennai. Patients with a strong correlation between impacted third molars and the IAC on digital OPG were selected for further analysis using CBCT. The study spanned one year from its approval by the Ethical Committee of Sathyabama University Dental College and Hospital.
The sample size calculation was based on a study by Balaji [1], used an effect size of 0.418, α = 0.05, and power = 0.90. Using G*Power software (3.1.9.3, Heinrich Heine Universität Düsseldorf, Germany), the required minimum sample size was 254 participants.
The inclusion criteria included patients of male and female participants aged 18-45 years with unilateral or bilateral mandibular third molar impaction who were randomly selected. The study targeted individuals of South Indian descent residing in the specified region.
Exclusion Criteria included individuals with systemic diseases or unwillingness to participate, patients with a history of mandibular injuries or surgeries, cases with diseases affecting jaw structure or development, incomplete clinical records or medical histories, mandibular third molars with incomplete root development.
Cone beam computed tomography (CBCT) scans were performed using the Carestream CS 9300 and CS 3D Imaging software to ensure consistency in imaging procedures. Linear measurements were calibrated using a millimetre-based set of known dimensions.
Orthopantomograms (OPG) were conducted using the Sinora ORTHOPHOS XG system with SIDEXIS imaging software.
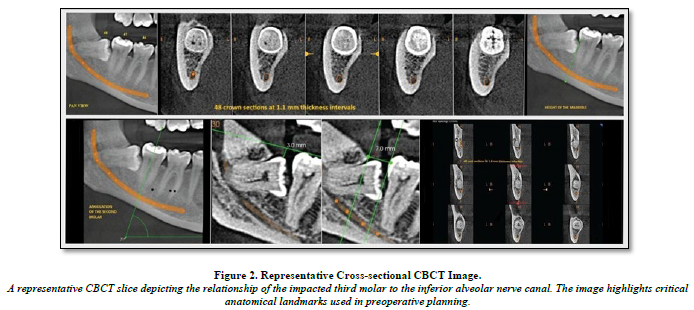
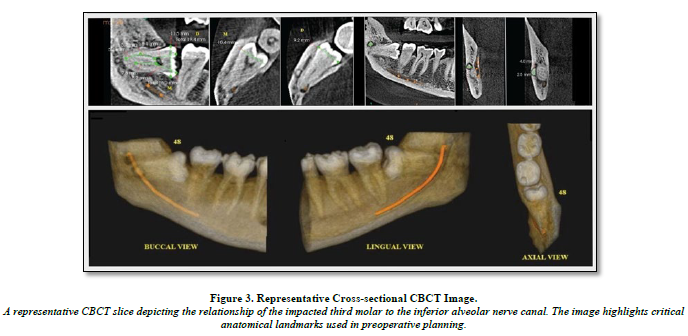
All participants underwent both OPG and CBCT imaging, with CBCT serving as the reference standard for evaluating impacted mandibular third molars. Unless otherwise noted, measurements were taken at the midpoint of the inferior alveolar nerve (IAN) canal in Figures 1-3.
Measured Parameters include:
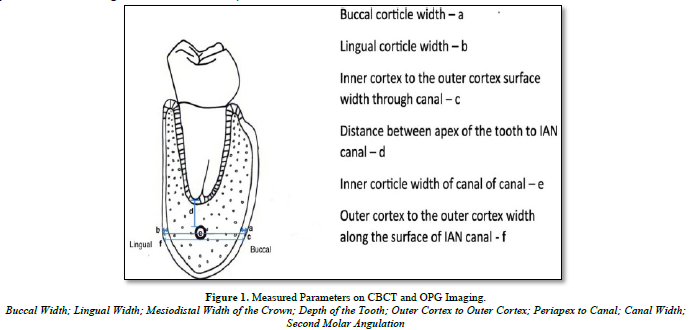
This figure illustrates various measured parameters used in the study for comparing OPG and CBCT images of impacted mandibular third molars, including buccal and lingual width, mesiodistal crown width, tooth depth, outer cortex-to-cortex distance, periapex-to-canal distance, canal width, second molar angulation, and height of the mandible.
Additional assessments include patient Details such as age, gender, molar angulation (left or right), Winter’s Classification: Horizontal, vertical, disto-angular, mesio-angular impactions, Wharfe Assessment like Height of the mandible, third molar angulation, root shape, follicle size, and path of exit. This study compared CBCT with OPG, focusing on parameters critical for preoperative evaluation and surgical planning.
DATA ANALYSIS
The Software used for statistical analysis is IBM SPSS version 21 (SPSS version 21.0; IBM corporation, Armonk, NY, USA). P-value of 0.05 thresholds of statistical significance was used. Normality test resulted in p-value less than 0.05. As a result, non-parametric tests were utilized for statistical analysis. Intergroup comparisons were conducted using the Mann-Whitney U test, while the Spearman rank correlation was applied to evaluate relationships between variables.
RESULTS
There were 254 people in the study who took part in the Wharfe assessment and comparative analysis of two imaging techniques: orthopantomogram (OPG) and cone beam computed tomography (CBCT). Statistical analysis showed that CBCT had a significantly higher mean score of 4.58 (SD 1.47) compared to OPG, as detailed in Table 1.
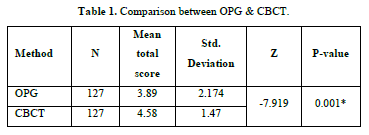
Above table shows the mean total score for CBCT (4.58) is higher than that for OPG (3.89), with standard deviations of 1.47 and 2.174, respectively, indicating lower variability in CBCT measurements. The statistical test yielded a Z-value of -7.919 and a P-value of 0.001, which is statistically significant (P < 0.05). This suggests that CBCT provides significantly better performance in this evaluation compared to OPG, reinforcing its higher accuracy and consistency in clinical assessments.
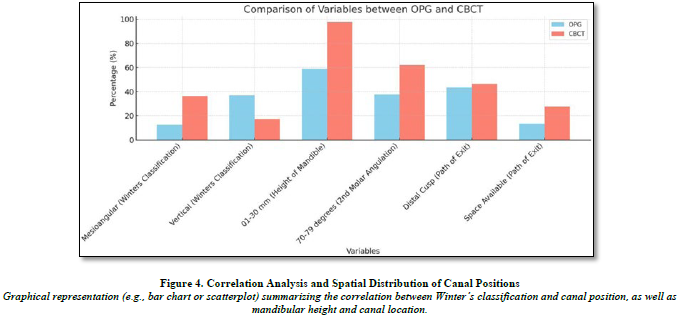
Table 2 demonstrates CBCT’s superiority over OPG in assessing impacted third molars, particularly in mandibular height measurement, second molar angulation, and path of exit evaluation, with statistically significant differences (P < 0.05). CBCT identified more cases within the 0-30 mm height range (97.6%), detected a higher percentage of 70-79 degree second molar angulation cases (62.2%), and provided better visualization of eruption space (27.6%). While CBCT and OPG showed no significant differences in Winter’s classification, root shape, or follicle size (P > 0.05), CBCT’s enhanced imaging capabilities allow for more precise assessments crucial for surgical planning. These findings reinforce CBCT’s role as a preferred diagnostic tool for impacted third molar evaluation.
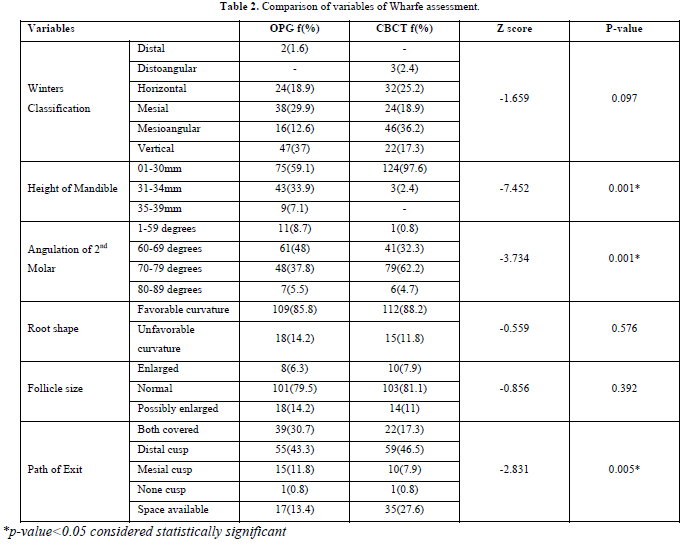
Table 3 presents the Spearman's rank correlation coefficients to assess the relationship between age, gender, and the total score based on the Wharfe assessment. The correlation between age and total score shows a significant positive relationship (r² = 0.187, P = 0.005), indicating that as age increases, the total score tends to increase as well, with a moderate strength of association. However, the correlation between gender and total score (r² = 0.001, P = 0.992) is negligible and statistically insignificant, suggesting no meaningful association between gender and the total score. Additionally, the correlation between age and gender (r² = 0.097, P = 0.146) is also weak and not statistically significant. Overall, age has a moderate and statistically significant correlation with the total score, while gender has no significant impact on the results.
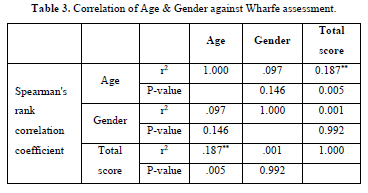
Table 4 presents the distribution of canal positions (buccal, central, and lingual) across different Winter’s classifications (distoangular, horizontal, mesial, mesioangular, vertical) in a total sample of 254 observations. The buccal position was most commonly associated with horizontal impactions (33.3%) and mesioangular impactions (29.2%), while the central position showed a higher frequency of vertical impactions (42.1%). The lingual position had the greatest frequency of mesioangular (38.9%) and vertical (28.2%) impactions. These findings suggest that the position of the canal is closely linked to the type of impaction, with the lingual position being the most common overall, contributing to 58.4% of the total sample. This distribution provides insights into the relationship between canal position and impaction types, which can help in surgical planning for tooth extractions. And, there were significant association seen between position of canal and winter’s classification with Pearson Chi-square value of 36.59, df (8) with p-value <0.05.
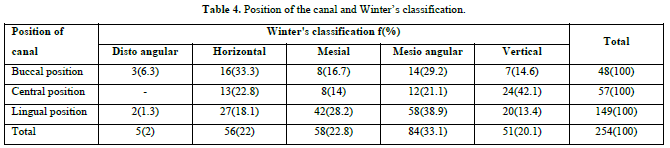
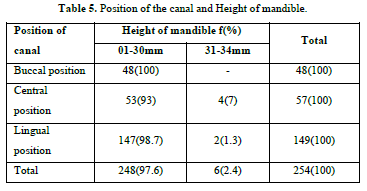
Table 5 presents the relationship between the position of the canal (buccal, central, and lingual) and the height of the mandible (categorized into 0-30 mm and 31-34 mm). The buccal position was exclusively associated with 0-30 mm height cases (100%), while the central position showed a majority in the 0-30 mm range (93%), with a small percentage (7%) in the 31-34 mm range. The lingual position was predominantly found in the 0-30 mm height range (98.7%), with only 1.3% of cases falling into the 31-34 mm range. Overall, the majority of cases (97.6%) were in the 0-30 mm range, highlighting that the lingual position is the most common canal position across both mandible height categories. This distribution is significant for understanding the anatomical variations in impacted molars and can aid in treatment planning, especially for surgical extractions. Also, there were significant association seen between position of canal and height of mandible with Pearson Chi-square value of 7.189, df (2) with p-value (Figure 4).
DISCUSSION
Various imaging modalities, such as periapical, panoramic, occlusal, conventional radiography, and computed tomography, are employed to pre-assess surgical sites. However, each technique has limitations. For posterior mandibular procedures, more precise diagnostic information may be needed to avoid critical structures like the IAN-MM complex, even though periapical radiographs of the anterior jaw often provide sufficient information. The front section of panoramic views is prone to overlap, and two-dimensional radiography cannot determine the exact location or thickness of vital structures in the buccolingual direction. Cross-sectional imaging techniques like magnetic resonance imaging (MRI) and various computed tomography (CT) modalities (spiral, linear, and hypocycloidal) have been used [8]. However, the high cost and radiation risks associated with these methods have drawn criticism [4]. As a result, CBCT was selected for this study over other techniques.
Reports suggest that CBCT is effective for imaging the craniofacial region. The primary goal of this study was to assess how CBCT compares to OPG in improving our understanding of risk factors. The mandibular canal typically appears as a well-defined radiolucent zone with radiopaque borders on CBCT. The radiographic density of this lucent structure varies, and the presence of a radiopaque outline depends on the canal's cortication [9].
The main focus of this study is to compare the accuracy of CBCT with OPG. CBCT’s three-dimensional nature allows more precise measurements of impacted teeth than OPG, improving the localization of the mandibular third molar in relation to the inferior alveolar nerve canal. Previous studies have found no significant differences between OPG and CBCT regarding parameters like mandibular height [22,23], second molar angulation [24,25], and the path of exit [26,27].
In comparing the Wharfe assessment variables between CBCT and OPG, the following findings were observed (Table 3):
Additionally, we correlated gender and age with the Wharfe assessment. Previous studies have noted gender-specific trajectories in the relationship between tooth eruption and jaw expansion [10]. Understanding gender differences related to impacted teeth is important. Research has shown a female predominance in the occurrence of impacted third molars [11-14], although some studies report no gender differences [15,16], which aligns with the findings of this study. Conversely, other studies have noted a male preponderance [17].
The Spearman’s rank correlation coefficient between gender and the Wharfe assessment is 0.146, indicating a very weak correlation. The significance level (Sig. 2-tailed) for this correlation is 0.992, which is much higher than the conventional threshold of 0.05 for statistical significance. Therefore, we conclude that there is no significant correlation between gender and Wharfe assessment in this study. These results indicate that gender does not have a statistically significant impact on Wharfe assessment outcomes.
Prior research has documented a relationship between age and Wharfe assessment, with impaction typically occurring in the second half of the third decade of life [18,19-21]. In this study, the results suggest a mild correlation between age and the Wharfe score.
While CBCT offers improved imaging capabilities, some studies suggest that it does not significantly correlate the position of the inferior alveolar canal (IAC) with Winter's classification, highlighting the need for further study to improve preoperative evaluation techniques [28,29]. On the other hand, other studies emphasize that understanding the significant associations between Winter’s classification and canal positioning through advanced imaging like CBCT can greatly enhance surgical planning and reduce risks associated with third molar extractions [35-37].
In our research, the distribution of cases by canal position (basal, central, lingual) and Winter’s classification (mesial, mesioangular, vertical, distoangular) is shown in Table 4. A Pearson Chi-square test reveals a significant correlation between the canal’s location and Winter’s classification, with a Pearson Chi-square value of 36.59, degrees of freedom (df) = 8, and a p-value
Some studies have found no significant spatial correlation between the IAC and mandibular height, suggesting that changes in mandibular height do not correlate with changes in the IAC position on CBCT [30]. However, other research has shown that mandibular height and the location of the IAC are significantly correlated, with CBCT proving more useful than OPG for accurately visualizing and determining these anatomical relationships.
In this study, the distribution of cases by mandibular height (01-30mm, 31-44mm) and canal position (lingual, buccal, or central) is shown in Table 5. The results demonstrate a significant correlation between mandibular height and canal location, with a Pearson Chi-square value of 71.89, df = 2, and a p-value
CLINICAL IMPLICATIONS
The notable variations in key parameters emphasize the benefits of CBCT over OPG, providing comprehensive details for complex surgical and dental procedures. CBCT is the preferred imaging method for accurate assessments, as it offers clear visualization of bone structures, tooth angles, and spatial relationships.
CONCLUSION
In conclusion, this study highlights CBCT’s superior diagnostic accuracy over OPG in assessing key parameters of impacted third molars, particularly mandibular height, second molar angulation, and path of exit evaluation (P < 0.05). CBCT identified significantly more cases within the 0-30 mm mandibular height range (97.6% vs. 59.1%, P < 0.001), allowing for more precise bone height measurements essential for surgical planning. It also detected a greater number of cases with significant second molar angulation (62.2% vs. 37.8%, P < 0.001), particularly in the 70-79-degree range, enhancing preoperative assessment for extractions. Additionally, CBCT provided improved visualization of distal cusp coverage (46.5%) and open space (27.5%) in the path of exit analysis (P = 0.005), aiding in predicting eruption patterns and surgical challenges. While no significant differences were found in root form or follicle size (P > 0.05), CBCT’s advanced imaging capabilities allow for more detailed anatomical assessments, including the correlation between canal position, mandibular height, and Winter’s classification. These findings strongly support the use of CBCT as a preferred imaging modality in clinical settings, as it provides highly accurate measurements and detailed three-dimensional visualization, ultimately improving treatment planning and patient outcomes.
No Files Found
Share Your Publication :